The ELDAC Residential Aged Care Toolkit: Assisting the transition to the Aged Care Quality Standards
A guest blog by Professor Deborah Parker, Professor of Aged Care (Dementia) and Dr Holly Mack, Research Fellow, Faculty of Health, University of Technology Sydney
Providing end-of-life care to residents with advanced life-limiting illnesses can be challenging for clinicians and health care workers. The ELDAC Residential Aged Care toolkit delivers a set of resources on person-centred palliative care and advance care planning to help you meet the complex care needs of residents and support their families.
The interactive toolkit is available online through the ELDAC website (www.eldac.com.au). The toolkit offers a comprehensive collection of information, resources and tools developed and reviewed by aged and palliative care experts. The Residential Aged Care toolkit is designed for direct care staff including nurses, care workers, allied health professionals and general practitioners (GPs), as well as staff in managerial, quality or educational roles. The toolkit can help users develop an evidenced-based plan and it is presented in a user-friendly format that is divided into three main sections: Clinical Care, Education and Learning, and Organisational Support.
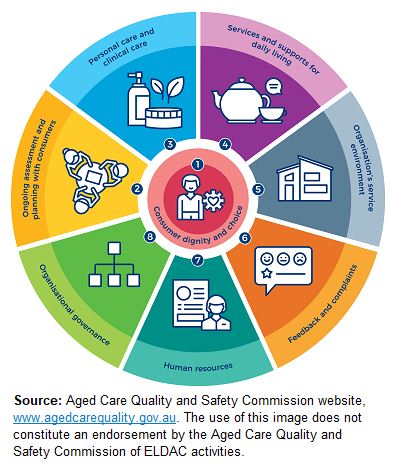 The Residential Aged Care toolkit can assist you and your organisation in meeting the eight Aged Care Quality Standards (see image to the left) that will be released on 1st July 2019. The standards apply to all aged care services including residential care. Each standard has three components: outcomes for the consumer; expectations for the organisation; and organisational requirements to demonstrate that the standard has been met. All of the standards have important implications for palliative care and four of the standards highlighted below are particularly relevant to those supporting advance care planning and working in end of life care. These are Standards 1, 2, 3, and 8.
The Residential Aged Care toolkit can assist you and your organisation in meeting the eight Aged Care Quality Standards (see image to the left) that will be released on 1st July 2019. The standards apply to all aged care services including residential care. Each standard has three components: outcomes for the consumer; expectations for the organisation; and organisational requirements to demonstrate that the standard has been met. All of the standards have important implications for palliative care and four of the standards highlighted below are particularly relevant to those supporting advance care planning and working in end of life care. These are Standards 1, 2, 3, and 8.
Standard 1 is about consumer dignity and choice. This standard underscores the importance of valuing diversity where every consumer should be treated with dignity and respect, especially in terms of their identity and culture. The Clinical Care section of the Residential Aged Care toolkit has materials on providing care that is culturally safe and offers information on supporting holistic care, including psychosocial and spiritual wellbeing. Throughout the Clinical Care section there are resources for different population groups including: religious and cultural backgrounds; people living with dementia; Aboriginal and Torres Strait Islander Peoples; and LGBTI groups. There are also resources for supporting families around communication, decision-making about care and involving others in their care.
The Work Together section of the toolkit highlights care coordination as essential and inclusive of all health professionals, the resident, and the family regarding care goals. Palliative care case conference information and templates are available to help document the multidisciplinary team meetings. Standard 2 focuses on ongoing assessment and planning with consumers. It explicitly identifies that this should include advance care planning and end of life planning, if the consumer wishes. The Advance Care Planning page of the Clinical Care section has general information and links to specific state/territory resources. There are resources to assist healthcare staff begin the conversation with residents about how they want to be cared for and what their wishes and preferences are for their end of life. The Clinical Care section offers person-centred clinical guidance across eight care domains and contains preferred assessment tools, forms and factsheets for assessing residents’ care needs.
Standard 3 is concerned with personal and clinical care so that a person’s needs, goals and preferences nearing the end of life are recognised and addressed. This includes consumers’ comfort being maximised and their dignity preserved and that staff recognise deterioration and respond in a timely manner. The Residential Aged Care Toolkit addresses these areas in the Recognise End of Life and Respond to Deterioration care domains. The toolkit recommends the Supportive and Palliative Care Indicators Tool (SPICTTM) to use for all residents during routine care evaluations in order to identify that someone may need end of life care. The SPICTTM is free and has user guidelines available.
Standard 8 is about embedding within organisational governance delivery of safe and quality care and services. The Organisational Support section of the toolkit promotes a multidisciplinary coordinated approach to assist your service in palliative care and advance care planning for residents and their families, and connecting with external services and forming partnerships. This section features the ELDAC Organisational and After Death Audits and the Advance Care Planning Continuous Quality Improvement Audit Tool.
The Education and Learning section of the toolkit offers an opportunity for you individually to evaluate your learning and development needs in providing end-of-life care with the ELDAC Personal Learning Assessment and create a Personal Learning Plan. There are links to online education modules to help you improve your knowledge, skills and confidence in palliative care and advance care planning.
The ELDAC Residential Aged Care toolkit connects people working in aged care with palliative care and advance care planning resources and services. The toolkit supports you and your organisation in identifying and addressing areas where residents’ outcomes can be improved in the transition to the Aged Care Quality Standards. Visit the toolkit regularly as we continue to deliver updates with the latest evidence-based information and develop new interactive resources.

Professor Deborah Parker, Professor of Aged Care (Dementia), Faculty of Health, University of Technology Sydney

Dr Holly Mack, Research Fellow, Faculty of Health, University of Technology Sydney