Why a Toolkit on Linkages?
Does your organisation have a goal of improving palliative care and advance care planning given to older people in your care who are near the end of life?
Do you believe that you could achieve these goals through working in partnership with other organisations rather than on your own?
Do you experience challenges in accessing other services to support the older people in your care who are near the end of life?
Perhaps you’ve come to the Linkages Toolkit because the provision of palliative care and advance care planning to the older persons in your care might be improved through working together with other services.
Older people can have multiple, complex illnesses as they near the end of their lives. This requires the input of range of health, aged and social care from a number of care providers – so palliative care is everyone’s business.
Achieving the best possible palliative care and advance care planning for older persons in your care doesn’t happen by chance. Providing this requires careful coordination and collaboration between these various services. This is a simple definition of partnership that applies to working together:
It is important to consider, though, that there is a range of ways of working together and not all of them represent partnering. This diagram shows how working with others can take many forms with a number of elements and varying benefits:
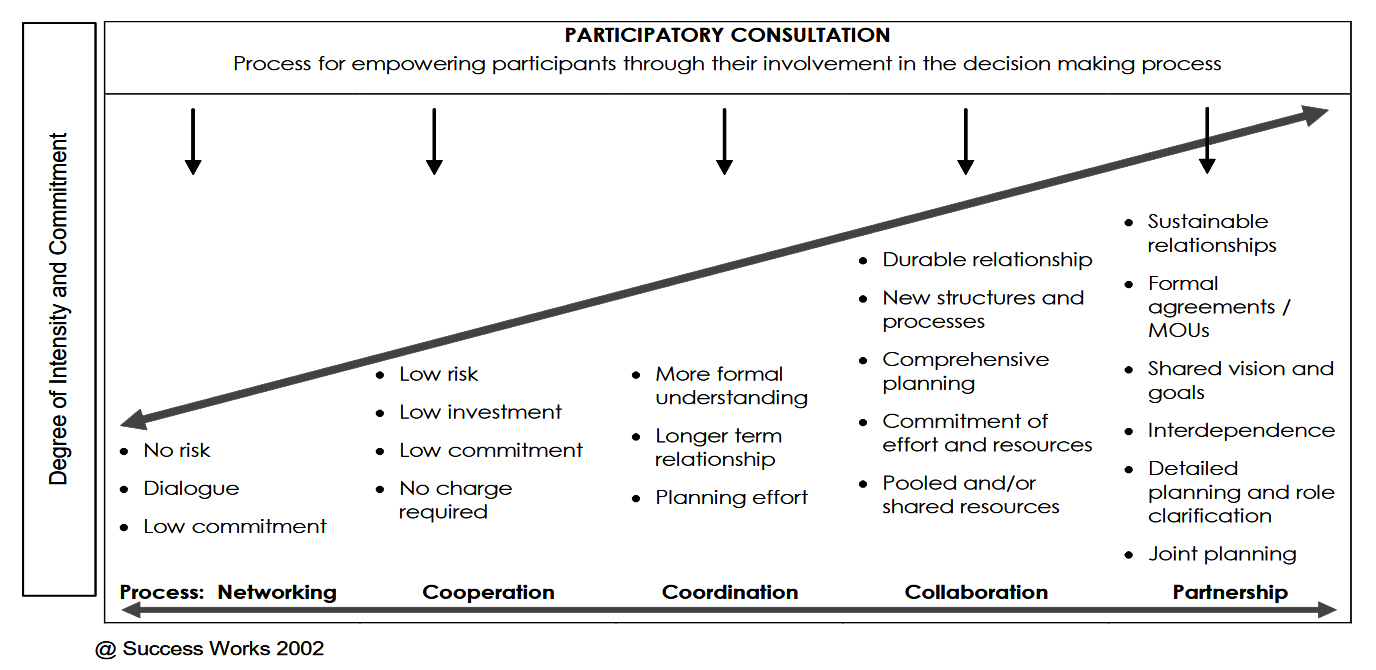
(Used with permission. https://www.synergistiq.com/)
Five principles of partnering that apply to this more deliberate way of working together are:
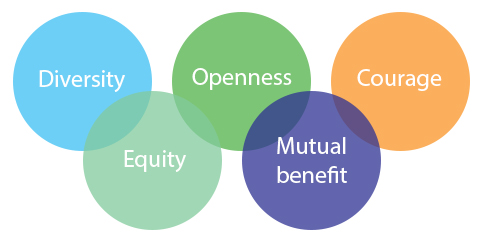
(From The Partnering Initiative https://thepartneringinitiative.org/)
In other words, entering partnerships to improve palliative care and advance care planning for older persons at the end of life is based on very deliberate strategies for working together. Partnering is a change management process for organisations and aligns with Continuous Quality Improvement processes that may already be in place in your workplace. It can impact on your outcomes at the individual, team, organisation and systems levels.
“Partnership is more than just collaboration on ad-hoc projects. It is about moving beyond responsibility for independent results, to a relationship that involves co-creation, shared risks and responsibilities, interdependency, and organisation transformation. True partnership is about identifying shared value and leveraging the combined strengths of each partner to achieve a level of impact that could not be accomplished independently.”
(KPMG, 2016: Unlocking the Power of Partnership.
https://assets.kpmg.com/content/dam/kpmg/pdf/2016/01/unlocking-power-of-partnership.pdf)(1.9MB pdf)
What is the evidence that working together in partnership between services helps improve palliative care and advance care planning for older people?
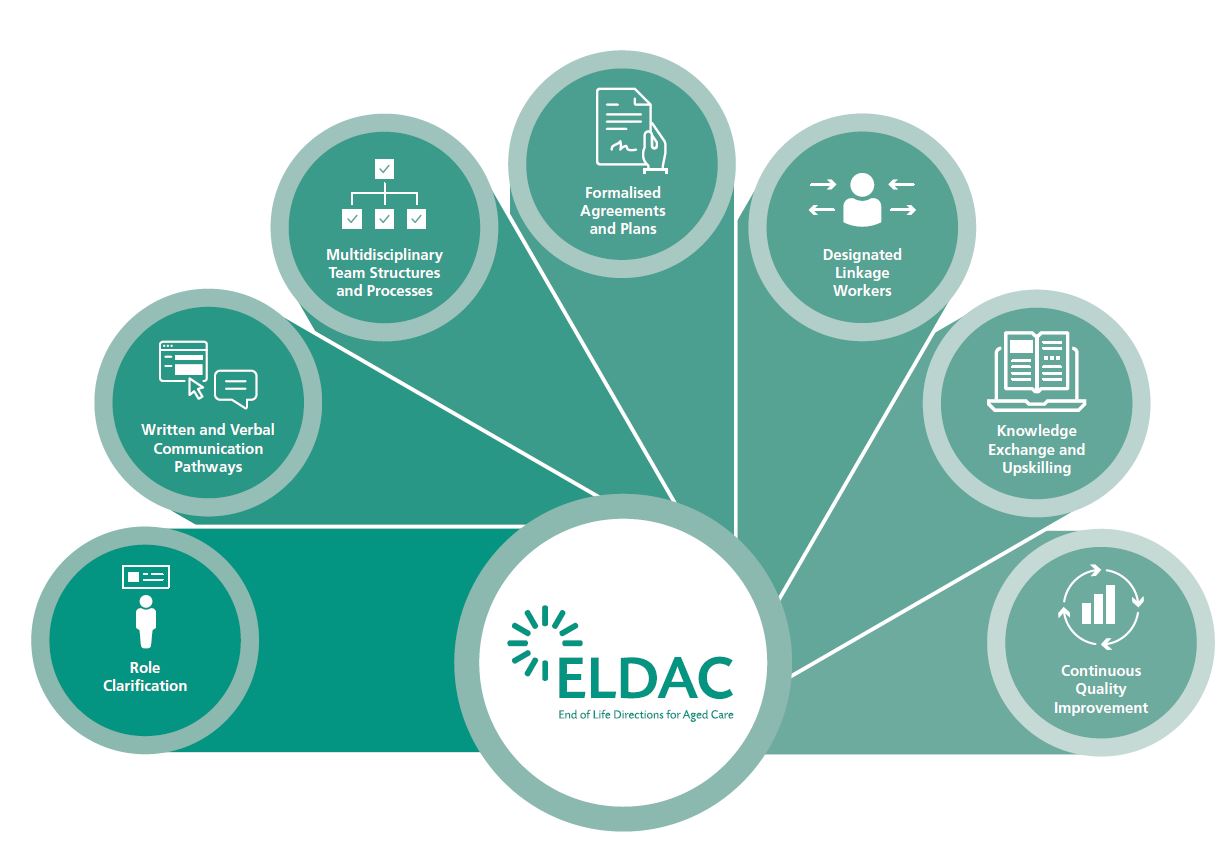
This toolkit has utilised the findings of the Decision Assist Palliative Aged Care Linkages project evaluation. An extensive systematic literature review was conducted and identified seven strategies for successful linkage between organisations:
Role clarification
Role clarification
Written and verbal communication pathways
Multidisciplinary team structures and processes
Formalised agreements and plans
Designated linkage workers
Knowledge exchange and upskilling
Continuous quality improvement
For an explanation of the seven strategies, you can view this short video.
The Linkages project trialled the implementation of these strategies in more than 30 sites across Australia, and positive changes to palliative care and advance care planning of older persons were widely reported. To assist with understanding the potential benefits of partnerships when providing palliative care for older people, see the real life case studies of how services like yours have implemented strategies to improve the collaboration between aged care and palliative care services.
As you work your way through this Toolkit, we recommend that you consider how each of these strategies might bring about the changes you seek in your care of older persons near the end of life.
It’s important to be clear about the terms we use in the care given to older persons at the end of life. Palliative Care Australia has introduced the following definitions to describe commonly used terms and these relate to this Toolkit.
What is advance care planning?
The process of preparing for likely scenarios near the end of life that usually includes assessment of, and discussion about, a person’s understanding of their medical condition and prognosis, values, preferences and personal and family resources. Advance care planning supports a person in communicating their wishes about their end of life.
What is palliative care?
Palliative care is an approach that improves the quality of life of patients and their families facing the problem associated with life-threatening illness, through the prevention and relief of suffering by means of early identification and impeccable assessment and treatment of pain and other problems, physical, psychosocial and spiritual.
What is a specialist palliative care service?
A multidisciplinary health care service whose substantive work involves consultative and ongoing care and support for people with a life-limiting illness, their carers and family. In general, specialist palliative care services would not be directly involved in the care of people who have uncomplicated needs associated with a life-limiting illness.
What is a primary care provider?
Health services and staff that have a primary or 'first contact'; relationship with the patient with a life limiting illness. The use of the term ‘primary care provider’ in this context refers to general practitioners (GP), community nurses, staff of residential aged care facilities (RACF) and multi-purpose centres. It also includes other specialist services. In general the substantive work of the primary care provider would not be with people who have a life limiting illness.
Read more.
Consider these practice areas within your organisation. Do you need to make changes in the way these are addressed?
- Advance care planning
- Recognising end-of-life care
- Assessing palliative care needs
- Providing palliative care
- Working together
- Responding to deterioration
- Managing dying
- Bereavement
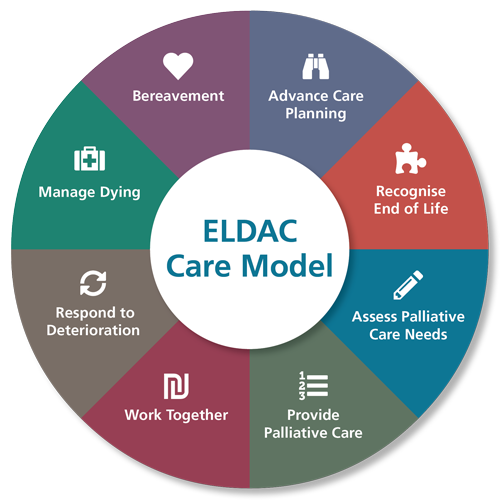
These are areas that you can effect change in through successful and sustainable partnerships when providing palliative care and advance care planning for older people. Depending on your particular settings of care, a number of ELDAC Toolkits may address these particular areas.
The Toolkit provides you with resources and links to other sites where you can find out more about working together to improve palliative care and advance care planning for older persons. Ideally, it can be used in conjunction with other ELDAC Toolkits although it can be used as a stand-alone resource.
When aged care providers and palliative care services work together, you can achieve:
- Fewer avoidable presentations to Emergency Departments during care at the end of life
- Shorter length of stay in hospital when residents/clients are admitted
- Improved quality of palliative care for older persons near the end of life in their usual place of residence
- Increased knowledge, skills and confidence in clinical care staff in providing palliative care
The ELDAC Linkages Toolkit has been created to help middle and upper level managers create partnerships between aged, primary and palliative care services. It takes you through the processes to establish and implement effective and sustainable partnerships between service providers.
Before you begin to work your way through this Toolkit, we recommend that you take a little time to understand the fundamental principles and practices of partnership development. The elements of the Linkages Toolkit are underpinned by elements of the partnering cycle. Many elements of partnering will be familiar already. You can see that the cycle is made up of four segments, each with its own components that step you through the information you need to establish and implement effective and sustainable partnerships between service providers.
Remember, whilst every partnership is unique, there is a great deal of similarity in how organisations work together in partnerships. The cycle shown here provides some guidance but does not represent a clear cut process – your path through these segments will rarely follow a linear path.
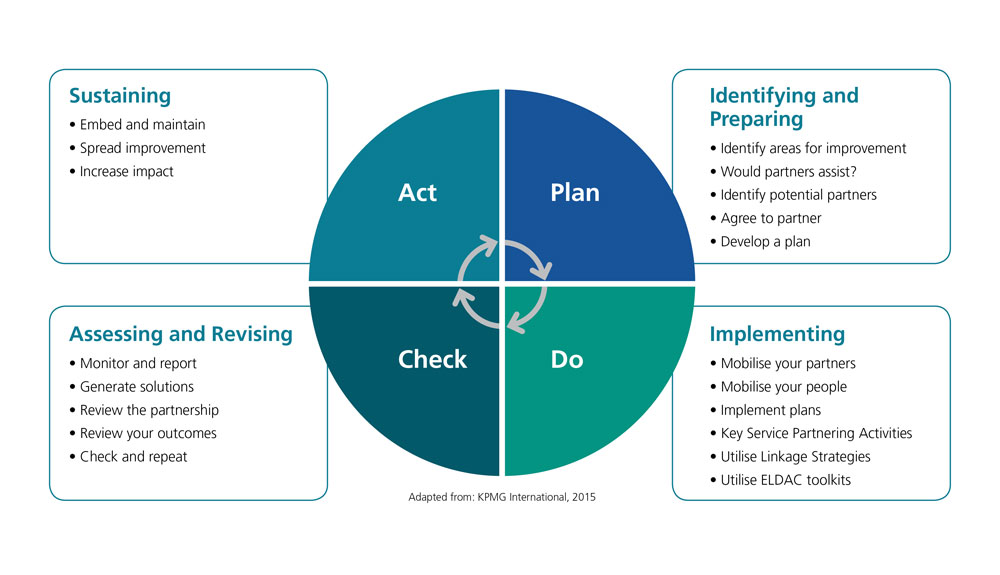
We do recommend, though, that you follow the steps within the Linkages Toolkit to systematically build the collaborations with others to achieve a successful and sustainable partnership when providing palliative care and advance care planning for older people. These steps are not necessarily linear – for example, strategies for evaluation and sustainability do not come at the end of this process; rather they are integrated throughout the whole process.
Working together in partnership is what this toolkit is all about.