Respond to Deterioration
Deterioration refers to signs of a person’s decline or reduced state of health. Being equipped to respond to deterioration quickly can:
- Ensure needs are reviewed and care is provided, according to preferences and values.
- Support commencement of a palliative care plan or pathway.
- Ensure appropriate management of symptoms, interventions and medications.
- Avoid unnecessary, unwanted or inappropriate transfers to hospital.
- Facilitate support for the older person and their family and carers.
Typical Illness Trajectories
Older people will experience different illness trajectories depending on their primary diagnosis and presence of other diseases (co-morbidities). Three typical illness trajectories for people with progressive chronic illness are described and illustrated in the figure below: [1, 2]
-
Trajectory 1
-
Trajectory 2
-
Trajectory 3
Trajectory 1: Cancer (short decline)
For these individuals there is a steady progression with a slight decline in physical health over months to years. Evident decline occurs in the end-of-life phase. This includes increasing symptoms, rapid decline in weight and functional status in the last weeks or months of life. [1, 2]
Trajectory 2: Organ failure (intermediate with acute episodes)
These individuals have non-malignant, life-limiting illness with organ failure. There is decline in function over years with long-term limitations, often life-threatening episodes requiring hospital treatment, followed by further deterioration. During this trajectory there may be episodes of improvement only for function to decline again. Death can seem sudden and may occur at any time along the gradual decline in function. [1, 2]
Trajectory 3: Frailty or dementia (gradual dwindling)
People living with dementia have a long and varied disease progression for up to 6-8 years. This includes early impairment of memory, reduced decision-making and communication capacity. Frailty is a syndrome of general physiological decline that often lacks a specific diagnosis. In this trajectory, the last year of life is characterised by a steady slow decline in overall function. If dementia and frailty occur together decline is more rapid. [1, 2]
Typical illness trajectories and palliative care phases towards the end of life
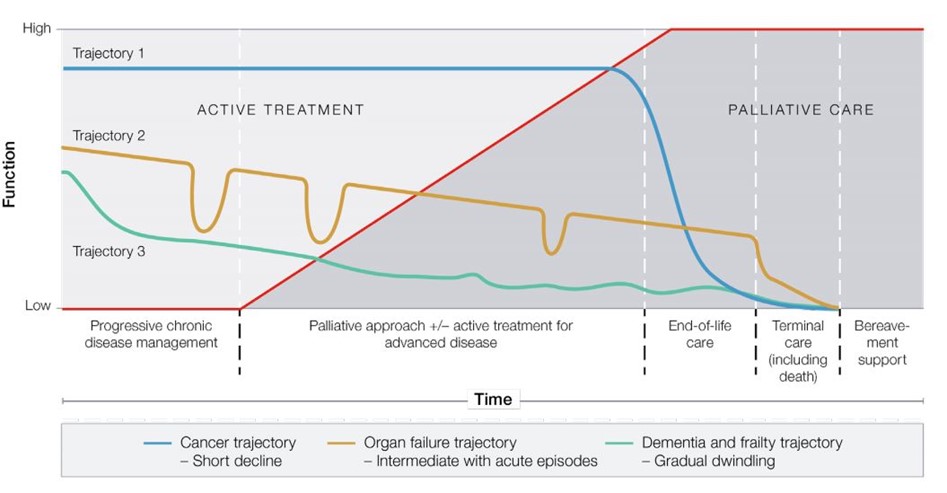
Reproduced with permission from: The Royal Australian College of General Practitioners. RACGP aged care clinical guide (Silver Book). 5th edition. East Melbourne, Vic: RACGP, 2019, 2020. Available at www.racgp.org.au/silverbook
It is important for clinicians and care workers to identify, plan, and be prepared to respond appropriately to deterioration across these illness trajectories. This may be caused by their primary diagnosis or as a result of other disease or events.
It is also important to distinguish between deterioration that is due to untreatable or irreversible causes like disease progression; and an acute or medical emergency that may be reversible, warrant review, and treatment. Good clinical assessment and consultation with the older person’s GP is critical. If needed, external experts should be contacted, such as specialist palliative care. Family and carers should also be contacted when an older person is deteriorating.
-
Signs of deterioration
-
Use tools to identify deterioration
-
Support continuity of care
Care workers may be the first to notice possible signs of deterioration, which may include:
- poor general health, such as wounds or increasing fatigue
- not returning to previous level of health after an illness
- reduced activity
- increasing falls
- needing additional help from others because of increasing health needs (physical or mental)
- losing weight over months, or remaining underweight
- unplanned emergency transfer/s to hospital.
The palliAGED Recognising deterioration in a resident short video clip provides a simple summary.
- The SPICTTM (184kb pdf) can be used during routine care evaluations and following an unplanned hospitalisation. It may indicate a change in an older person’s condition that warrants a review of care needs. Refer to the RAC Toolkit Recognise End of Life section for further information.
- The Stop and Watch Early Warning Tool (481kb pdf) can be used by care workers to spot signs of deterioration in older people. The tool can be used in situations of increased concerns when team members notice that something isn’t quite right.
Supporting continuity of care will include:
- Accessing after hours medical care to ensure appropriate care at all times. In some states and territories acute hospital services have rapid response teams that may offer phone support or provide consultation. Similarly, in some states and territories extended care paramedics may be available.
- Enacting decision-making that is guided by the older person’s preferences and values. These can be expressed in an advance care plan or Advance Care Directive.
- Ensuring clinical information accompanies the older person in the event that an emergency department presentation and/or hospital admission is required. This includes legal documents identifying substitute decision-makers, advance care plans or an Advance Care Directive.
- Liaising with the hospital following transfer to support the older person’s return if their condition stabilises (dependent on their preferences). If you are able to provide the care required for the older person, discuss this with the hospital staff. For more information, palliAGED has Practice Tips on continuity of care for Nurses (225kb pdf) and Careworkers (337kb pdf)).
ACP documents may be kept with the person, substitute decision-maker(s), their GP, or the residential aged care provider.
In residential aged care, Advance Care Directives/Planning documents should be:
- be stored safely
- be accessible to team members and other visiting service providers involved in decision-making about care
- accompany an older person when transferred to hospital.
Refer to your own organisation’s policies and procedures when considering how to manage Advance Care Directives/Planning documents within your setting. Support the older person in nominating an authorised representative to upload their ACP documents to My Health Record. This portal can be securely accessed when needed.
- Gain a better understanding about delivering palliative and end-of-life care by listening to the ELDAC podcast series 'The What to do, When and How'.
- Watch the ELDAC Residential Aged Care Toolkit Manage Dying educational video. It also discusses how to respond to an older person in residential care who is declining in health.
- Read the palliAGED Practice Tips on:
- Complete the palliAGED online learning module on Recognising deterioration.
- Know the options for after-hours support to be well prepared if an older person in your care requires emergency review. Undertake a simple quality improvement activity to map local options for after-hours support and consultation. These options may include rapid response teams or extended care paramedics.